Over 1 billion people worldwide have a vitamin D deficiency.
Difficulties with memory and learning are signs of vitamin D deficiency, research finds.
Vitamin D deficiency is even linked to disorders such as depression and schizophrenia.
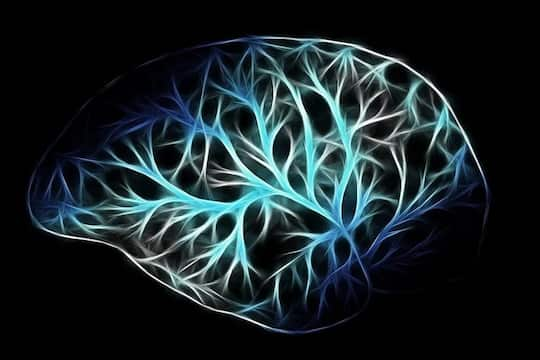
Deficiency in the vitamin affects critical structures in the hippocampus, an area of the brain important in memory and learning.
Dr Thomas Burne, study co-author, said:
“Over a billion people worldwide are affected by vitamin D deficiency, and there is a well-established link between vitamin D deficiency and impaired cognition.
Unfortunately, exactly how vitamin D influences brain structure and function is not well understood, so it has remained unclear why deficiency causes problems.”
For the study, researchers removed vitamin D from the diets of mice for 20 weeks.
The mice clearly showed problems with learning and memory compared to a control group, who were fed sufficient levels of vitamin D.
The researchers found that vitamin D is important in keeping perineuronal nets in the hippocampus stable.
Dr Burne explained:
“These nets form a strong, supportive mesh around certain neurons, and in doing so they stabilise the contacts these cells make with other neurons.
As neurons in the hippocampus lose their supportive perineuronal nets, they have trouble maintaining connections, and this ultimately leads to a loss of cognitive function.”
The hippocampus is a particularly active part of the brain, which may be why it is affected by vitamin D deficiency early on, said Dr Burne:
“It’s like the canary in the coalmine—it might fail first because its high energy requirement makes it more sensitive to the depletion of essential nutrients like vitamin D.
Intriguingly, the right side of the hippocampus was more affected by vitamin D deficiency than the left side.”
The damage to these perineuronal nets may help to explain the memory problems that are a symptom of schizophrenia.
Dr Burne said:
“The next step is to test this new hypothesis on the link between vitamin D deficiency, perineuronal nets and cognition.
We are also particularly excited to have discovered these nets can change in adult mice.
I’m hoping that because they’re dynamic there is a chance that we can rebuild them, and that could set the stage for new treatments.”
The study was published in the journal Brain Structure and Function (Al-Amin et al., 2019).