Awe and wonder can help people feel more connected and reframe problems.
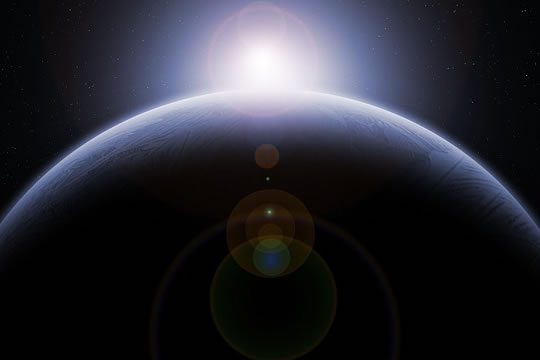
Astronauts who see the Earth from space could provide a clue as to how we can all feel more awe and wonder, new research suggests.
The view from so far away from the Earth provokes a special phenomenon called the overview effect.
Dr David Yaden, the study’s first author, said:
“We watch sunsets whenever we travel to beautiful places to get a little taste of this kind of experience.
These astronauts are having something more extreme.
By studying the more-extreme version of a general phenomenon, you can often learn more about it.”
The researchers analysed the reports of many astronauts from all over the world.
Each had documented their own experience of seeing the Earth from space for extended periods.
They frequently described it as a life-changing experience.
They mentioned ideas like connectedness, vastness, perception and unity.
Despite the religious or spiritual overtones, the experience was very secular for the astronauts, Dr Yaden explained:
“Space is so fascinating because it’s a highly scientific, highly secular environment, so it doesn’t have these connotations.
We think of people who do a lot of meditation or climb mountains, people who are awe junkies, having these experiences.
We don’t [often] think of these very strict scientists reporting these blissful moments.”
The astronauts’ experience is so fascinating — and potentially life-changing — that the researchers want to find out how we can all have more of it in our lives.
Mr Johannes Eichstaedt, one of the study’s co-authors, said:
“Behavior is extremely hard to change, so to stumble across something that has such a profound and reproducible effect, that should make psychologists sit up straight and say:
‘What’s going on here?
How can we have more of this?'”
The researchers are planning a follow-up experiment which will give people the opportunity to gaze at the Earth from space in virtual reality.
Perhaps it will be a life-changing experience — just as it is for the astronauts.
The study was published in the journal Psychology of Consciousness (Yaden et al., 2016).