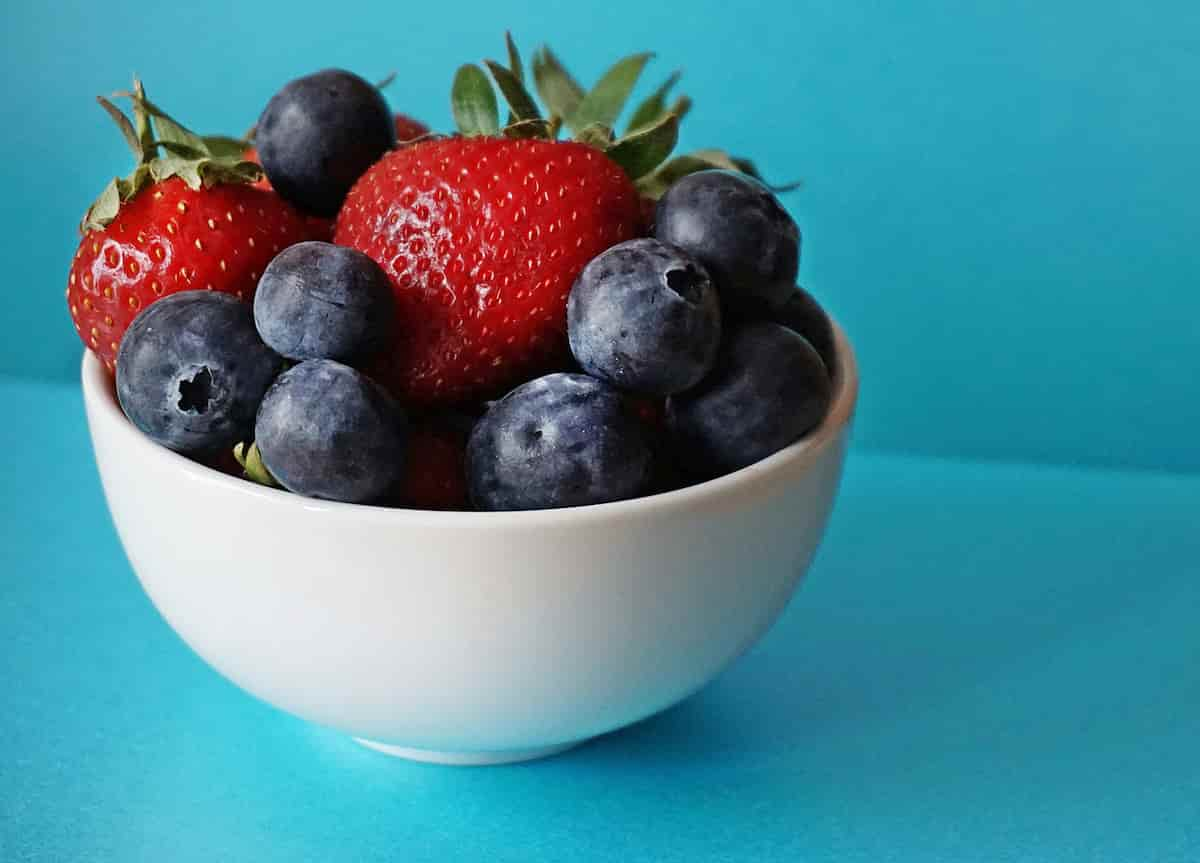
The types of fruit that can reduce cognitive aging and lower the risk of Alzheimer’s in midlife.
Daily consumption of strawberries or blueberries may lower the odds of dementia and Alzheimer’s disease in middle-aged men and women.
According to a study, both strawberries and blueberries contain effective antioxidants that help prevent the risk of late-life dementia.
Midlife adults can get the optimal health effect if consuming at least one cup of whole strawberries or blueberries per day.
Anti-aging antioxidants
A group of antioxidants called anthocyanins are responsible for the red, purple, or blue pigments of fruits and flowers.
Studies show that these antioxidants, due to their anti-inflammatory effect, can lower the risk of heart disease, type-2 diabetes and cancer.
Berries are rich in anthocyanins and several nutrients such as ellagic acid, that is known for its anti-aging effects, improving memory and other cognitive skills.
Professor Robert Krikorian, the study’s first author, said:
“Both strawberries and blueberries contain antioxidants called anthocyanins, which have been implicated in a variety of berry health benefits such as metabolic and cognitive enhancements.
There is epidemiological data suggesting that people who consume strawberries or blueberries regularly have a slower rate of cognitive decline with aging.”
Slow cognitive decline
Around half of the American adult population with prediabetes are middle-aged.
This group are more vulnerable to memory loss and cognitive decline.
Past research has suggested that eating strawberries can boost cardiovascular health by improving insulin sensitivity and lowering blood glucose levels.
This study investigated whether strawberry consumption provides any health benefit in overweight middle-aged individuals with self-reported cognitive decline.
Professor Krikorian said:
“This study assessed whether strawberry consumption might improve cognitive performance and metabolic health in this population, and if so, whether there might be an association between cognitive enhancement and reduced metabolic disturbance.”
One cup of strawberries
The participants in this study received every day a sachet of strawberry powder, equal to one cup of whole strawberries, for 3 months.
During the study period, the participants took various tests to measure their cognitive abilities such as long-term memory, as well as their emotional state such as mood, anxiety, and depressive symptoms.
The strawberry-treated group experienced a significant reduction in memory interference.
Professor Krikorian said:
“Reduced memory interference refers to less confusion of semantically related terms on a word-list learning test.
This phenomenon generally is thought to reflect better executive control in terms of resisting intrusion of non-target words during the memory testing.”
Furthermore, the strawberry-treated participants also experienced less depressive symptoms.
Professor Krikorian said the positive effects can be due to:
“…enhanced executive ability that would provide better emotional control and coping and perhaps better problem-solving.”
Lowering brain inflammation
Other studies have found that higher consumption of strawberries improves metabolic measures such as lowering insulin levels.
Professor Krikorian pointed out:
“Those studies generally used higher dosages of strawberry powder than in our research, and this could have been a factor.”
It seems the improvement of cognitive function by eating strawberries could be due to decreased brain inflammation.
Professor Krikorian said:
“Executive abilities begin to decline in midlife and excess abdominal fat, as in insulin resistance and obesity, will tend to increase inflammation, including in the brain.
So, one might consider that our middle-aged, overweight, prediabetic sample had higher levels of inflammation that contributed to at least mild impairment of executive abilities.
Accordingly, the beneficial effects we observed might be related to moderation of inflammation in the strawberry group.”
Related
- One cup of cranberries a day reduces the risk of neurodegenerative disorders.
- Lingonberry juice lowers blood pressure in the long-term.
- Flavonoid-rich foods can reduce blood pressure levels.
- Blackcurrants are found to improve mood.
The study was published in the journal of Nutrients (Krikorian et al., 2023).