Amyloid proteins may not be the cause of Alzheimer’s after all.
The real cause of Alzheimer’s is a dysfunctional ‘tau’ protein, a new study of over 3,600 brains finds.
Amyloid, a toxic protein frequently linked to Alzheimer’s may not be the main driver of the disease after all.
The tau protein normally helps stabilise the brain’s structure.
The fight against Alzheimer’s should be focused on the tau protein from now on, the researchers think.
Dr Melissa Murray, a neuroscientist at the Mayo Clinic in Jacksonville, and one of the study’s authors, said:
“The majority of the Alzheimer’s research field has really focused on amyloid over the last 25 years.
Initially, patients who were discovered to have mutations or changes in the amyloid gene were found to have severe Alzheimer’s pathology — particularly in increased levels of amyloid.
Brain scans performed over the last decade revealed that amyloid accumulated as people progressed, so most Alzheimer’s models were based on amyloid toxicity.
In this way, the Alzheimer’s field became myopic.”
The research looked at 3,618 brains stored in the Mayo Clinic.
1,375 had confirmed Alzheimer’s and had died at different ages, providing a timeline of the disease’s progression.
Dr. Murray explained:
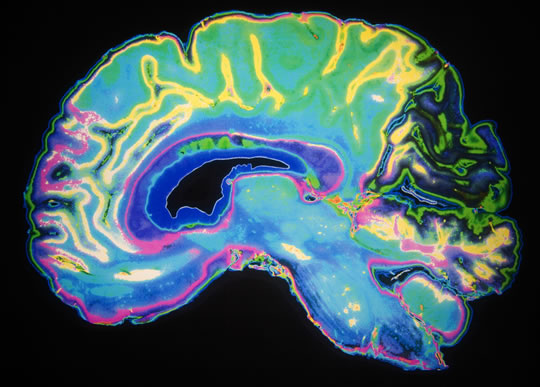
“Imagine looking at the rings of a tree — you can identify patterns, like the changing seasons and the aging of the tree, when viewing the tree’s cross-section.
Studying brains at different stages of Alzheimer’s gives us a perspective of the cognitive impact of a wide range of both amyloid and tau severity, and we were very fortunate to have the resource of the Mayo brain bank, in which thousands of people donated their postmortem brains, that have allowed us to understand the changes in tau and amyloid that occur over time.”
The researchers found that it was the tau protein, not amyloid, that predicted the onset of cognitive decline.
Dr. Murray explained the importance of the tau protein:
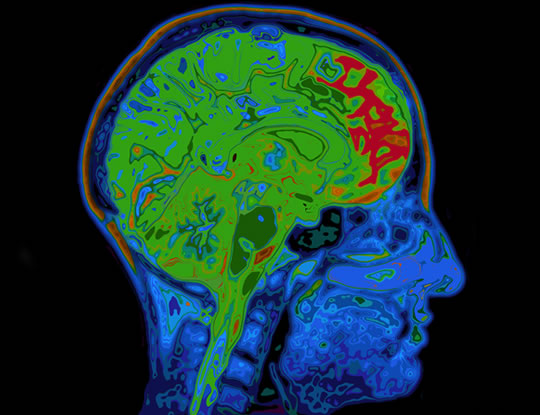
“Tau can be compared to railroad ties that stabilize a train track that brain cells use to transport food, messages and other vital cargo throughout neurons.
In Alzheimer’s, changes in the tau protein cause the tracks to become unstable in neurons of the hippocampus, the center of memory.
The abnormal tau builds up in neurons, which eventually leads to the death of these neurons.
Evidence suggests that abnormal tau then spreads from cell to cell, disseminating pathological tau in the brain’s cortex.
The cortex is the outer part of the brain that is involved in higher levels of thinking, planning, behavior and attention — mirroring later behavioral changes in Alzheimer’s patients.
Amyloid, on the other hand, starts accumulating in the outer parts of the cortex and then spreads down to the hippocampus and eventually to other areas.
Our study shows that the accumulation of amyloid has a strong relationship with a decline in cognition.
When you account for the severity of tau pathology, however, the relationship between amyloid and cognition disappears — which indicates tau is the driver of Alzheimer’s,”
The study is published in the journal Brain (Murray et al., 2015).
Alzheimer’s photo from Shutterstock