The everyday changes that could save you from dementia.
1. Follow the MIND diet
A new diet could lower the risk of developing Alzheimer’s disease by over 50%, a study finds.
It is known as the ‘MIND diet’, which stands for Mediterranean-DASH Intervention for Neurodegenerative Delay.
It is a combination of a Mediterranean diet and a diet developed for cardiovascular health (DASH: Dietary Approaches to Stop Hypertension).
Here are the ten “brain-healthy food groups”:
- Green leafy vegetables,
- other vegetables,
- nuts,
- berries,
- beans,
- whole grains,
- fish,
- poultry,
- olive oil
- and wine.
More details of the diet are here.
2. Avoid air pollution
Living further away from major roadways has been linked to better brain health by new research.
Long-term exposure to even moderate levels of air pollution, the study found, is bad for the brain.
Air pollution may cause poor cognitive function and ‘silent strokes’, which have been linked to dementia.
The study also found that people exposed to more air pollution had smaller brains.
3. Drink some alcohol…but not too much
For people over 60, light or moderate alcohol intake is associated with better recall of past events, according to a recent study.
Links were also found between increased size of the hippocampus — the area of the brain crucial to memory — and moderate alcohol consumption.
4. Get enough vitamin D
Low levels of Vitamin D are substantially associated with developing Alzheimer’s and dementia in older people, according to the best study conducted so far.
An international team of scientists used data from 1,685 elderly Americans who were followed for around five years (Littlejohns et al., 2014).
Those low in Vitamin D were 53% more likely to develop dementia.
Amongst those who were severely deficient, the risk increased by 125%.
Similar increases in risk were seen for Alzheimer’s disease: low levels of vitamin D increased risk by 69% and severe deficiency by 122%.
5. Remain calm
Anxiety, jealousy and moodiness in middle age are associated with doubling the risk of developing Alzheimer’s, a recent study found.
The study followed 800 women for 38 years and looked at the effects of their neuroticism on the chance of developing dementia.
Neuroticism is a personality trait that includes moodiness, worrying and anxiety.
In general, people who are neurotic are more likely to be anxious, depressed, jealous or envious.
More neurotic women who were under high levels of stress were more likely to develop Alzheimer’s disease.
6. Sleep well…
Poor sleep is a channel through which Alzheimer’s disease can be triggered, a new study finds.
Professor Matthew Walker, one of the neuroscientist who authored the study, said:
“Sleep is helping wash away toxic proteins at night, preventing them from building up and from potentially destroying brain cells.
It’s providing a power cleanse for the brain.
[…]This discovery offers hope.
Sleep could be a novel therapeutic target for fighting back against memory impairment in older adults and even those with dementia.”
7. …and get slow-wave sleep
Spending less time in slow-wave or deep sleep is linked to the loss of brain cells that can lead to dementia, a new study finds.
Slow-wave sleep, which occurs mostly in the first three hours of the night, is when the brain processes thoughts and memories.
The results also showed that those who got the most slow-wave or deep sleep performed better on tests of both thinking and memory.
8. Small amount of exercise
A relatively small increase in exercise is enough to boost brain function in older adults, a new study finds.
The amount of exercise that’s beneficial is equivalent to a brisk 25-minute walk several times a week.
Healthy over-65s who exercised more had better attention and ability to focus, the research found.
Professor Jeffrey Burns, co-director of the Kansas University Alzheimer’s Disease Center, said:
“Basically, the more exercise you did, the more benefit to the brain you saw.
Any aerobic exercise was good, and more is better.”
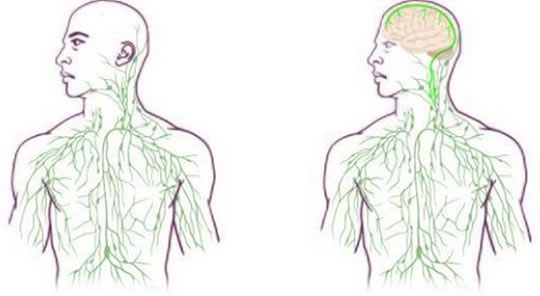
Brain image from Shutterstock